 There is a saying that goes, "When one door closes, another opens." I'm sure you have heard it. It is a quote that is used often when dealing with difficult situations and for some experiences, it can inspire. But how do you find an open door when your baby is struggling to live and their fate is out of your hands? How do you hold onto hope for tomorrow in the darkest hours of your life? And what if the day comes when your baby slips away?  The NICU is a place where you will find moments of pure unimaginable tragedy. Memories of mothers holding their babies against their chest for the last time; of fathers clutching their newborn's hands in their final hours. When I think of our NICU experience, I can almost hear myself sobbing and screaming "not my baby, no, no no..." But I still will always argue, that an open door can be found in the NICU. That indeed, even when tragedy occurs, hope may be found. Hope is found in memories of the first time you laid eyes on your little one, in your new found family of health professionals dedicated to your baby's care, in the quiet moments of the night when you watch over your little one as he sleeps, and in milestones both big and small. The NICU is a place that no parent would ever want their child to start his or her life in. However, it is the only place you would want your child to be if their first day is their hardest. It offers quality care and technologies that will give your baby the best chance as they fight for their life. But in those first moments in the NICU, many doors close; your dreams for a healthy baby, a perfect bonding experience after delivery and overall, your own peace of mind. It might seem that the opportunities for your dreams to come true are over. It can be devastating as you watch those old dreams crumble. On a bad day in the NICU it can get increasingly more difficult to find new open doors; new dreams to motivate you. On a good day you might be able to see through the haze of deep grief and and find new hope in a tomorrow for your family, in milestones met and for that one sweet day when you will finally take your baby home. If the day does come when you must say goodbye to your little one, all doors may seem to close. But tomorrow is still waiting for you. New aspirations will be found: dreams to honor the life and legacy of your baby, a hope found in the memories that surround you of your baby, opportunity in a new outlook in life and comfort in the warmth of loved ones. These new found dreams do not negate your journey. It does not mean that you do not grieve the life that you once had. These dreams are a catalyst to help you embrace life in the NICU and in life after. New dreams are symbolic of your strength, determination and courage to love and live another day. The NICU will always be a place of beginnings and of ends. It is a space where dreams come to light, dreams are diminished and new dreams can take wing. Never lose hope, there will always be another day and with tomorrow, an open door may wait. "When one door closes, another opens: but we often look so long and so regretfully upon the closed door that we do not see the one which has opened for us." -Alexander Graham Bell Written by Sarah King. Sarah is the mother of two children. Her first born child lost his fight in the NICU. She gives back to her community in his honor. Sarah currently serves as President at Project Sweet Peas. Learn more about Project Sweet Peas at www.projectsweetpeas.com
pPROM Statistics
by Krystal Roark Originally featured on Mommy of Twin Angels ***Warning*** If you have just experienced pPROM, or are currently on bed rest from pPROM I suggest you not read the blog entry below, unless you can pull yourself far enough out of the equation that it does not diminish your hopes. If you are like me and can do this, information is helpful (even when it is grim). pPROM, or premature rupture of the membranes, is largely looked at as a rare occurrence. When pregnant you are told your chances of miscarriage before the 12th weeks of gestation are range from 75% – 5% based on the gestational week (see chart below). Once you surpass the 12 week mark your chances of miscarriage drop significantly to less than 3%.6 Most women know this fact, or are made aware of it at the time of pregnancy. This is why many women wait until after 12 weeks to announce their new bundle of joy on the way. My question is, why are we never made aware of pPROM? Until it happened to me, I didn’t know it existed. After speaking with other women, a mix of those who have themselves experienced pPROM and those who have not, the general consensus is that they were unaware of its occurrence as well. I conducted a poll, in which 67 women responded. Of those 67 women, approximately 88% were unaware you could even have your water break before a term delivery. Of those who were aware, many worked in the medical profession. After my loss, I joined a group of over 500 women who have experienced pPROM, and subsequently lost their child/ren. This got the old scientifically trained brain wondering. Just how many women are affected by this? So, I did what I love to do. I researched the topic. Below you can read my findings. Before I start in though, I want to stress that I am NOT a doctor, nor am a professional in any field related to pPROM. This is purely my own small sample of research. First I decided to research miscarriage. Of women who find out that they are pregnant, usually around 4-6 weeks pregnant, 12 % will end in a miscarriage. This equals out to be somewhere in the range of 1 out of 8 pregnancies in the US. This percentage, unfortunately, is much higher in those who do not ever find out that they are pregnant. Usually those pregnancies are chalked up to a late period.6 So, what about pPROM? pPROM occurs somewhere in the range of 3-5% of pregnancies in the US and accounts for around 25-40% of all preterm deliveries.3,1 More than 140,000 pregnancies annually are complicated by pPROM and is the primary contributor to perinatal morbidity and mortality.1 It is a sad fact that even with immediate assistance at a hospital, those women who are in their 2nd trimester have between a 50-60% chance that they will go on to deliver their baby (usually before the gestational age of viability) within 1 week of rupture.4 With my twins, I beat the odds, and went on to have 7 weeks of bed rest before a c-section was scheduled due to a suspected infection (which turned out to be nothing and I could have carried them longer). When I questioned many doctors about pPROM and management, many times I was given different answers. There was no general consensus. Even asking on my support group, women were given much different answers by each doctor. Why is this? I found a study conducted that surveyed 508 different MFM (Maternal Fetal Management) providers that represented all 50 states and covered 13 countries. Of those 508 providers, only 30% reported that they had a formal departmental protocol for management of those women who experience pPROM. This seems unacceptable to me. Quick decisions are what could possibly save the life of these tiny babies still trying desperately to grow! The most commonly used protocols were steroids (99.4%) and antibiotics (99.6%). Both of which I was immediately put on in the hospital when I ruptured. After the initial dose of steroid shots, repeated dosing was uncommon at only 16%. This is due to research that confirms multiple dosing shows no significant advantage in lung development.7 So, why did I put this out there? I want to raise awareness. If you have experienced pPROM, do your research and make sure you are getting the best possible treatment. Take your management plan into your own hands; ask questions, why are you choosing not to do this or that? I did. Likelihood of miscarriage by Gestational age2 Weeks: 1-2 (before missed period) : 75% – This includes fertilized eggs that never implanted 3-6 : 10% 6-12 : 5% 2nd trimester : 3% 3rd Trimester – This is no longer considered a miscarriage, but a still birth (usually beyond 1 lb and 24 weeks of gestational age)
 August 26th, 2013 Rhea Selena DiBernardo was born 15 weeks early. She was 13 inches long and weighed 1 lb. 10 oz. She spent 3 months in the NICU at Magee Women's Hospital, located in Pittsburgh Pa. We visited her every day, and on day 27 we were able to hold her for the first time. She had several scares with infections, had her feedings stopped and started, and there were many days of weight gains and losses. Rhea had several blood transfusions and x-rays during her stay in the NICU. She was released to our care one week before Thanksgiving, but only came home for one day, as she ended up going to Children’s Hospital for a week resulting from a cold. Rhea finally ended up coming home the beginning of December, and thrived at home and is now 15 lbs, smiling at everything, and has just started crawling. Throughout our stay at Magee we emotionally survived by the kindness of friends and co-workers, the patience, support, and information from all of the staff at the hospital. We made friends with other families in the NICU who we still currently talk to; and it helped us to cope with the stressful times. Small gifts such as toys and blankets gave normalcy to our daughter's birth.  We wanted to reach out to other families who are currently going through what we already have experienced. We hope the story of Rhea will give comfort in a time that does not make sense. She has an optimal story of successes with few setbacks. There are many factors we attribute to the success of Rhea, which were the decisions made by the medical staff, and we know we have been lucky. In honor of Rhea’s first birthday we organized a fundraiser with Magee Womens Hospital and Bob Evans to support other families starting their journey in the NICU and to give thanks to Magee for the wonderful care Rhea received while she stayed there. Every Saturday in September 15% of a meal purchased at Bob Evans will go to the NICU fund, all you need is to show is the flyer either in hand or on your mobile device to participate. All Southwest PA stores and surrounding Pgh stores are participating! My son's name is Bryce and during our 18th week of pregnancy, we learned that he had a complete bilateral cleft lip and more than likely palate. It's known to be a very common birth defect throughout the word. Bryce doesn't use a special nipple however we did start out with the mead johnson bottle but now we do not. He also doesn't have reflux like it is projected with cleft babies. However, he does have other health problems. Our nicu stay lasted for 33 long agonizing days of cranial iv's, blood transfusions, and so much more. Bryce is very strong baby and I wouldn't change a thing.
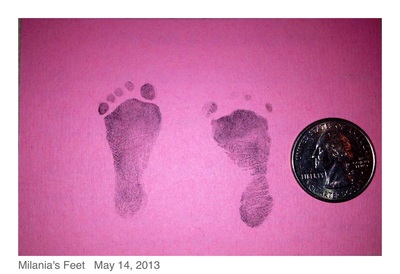
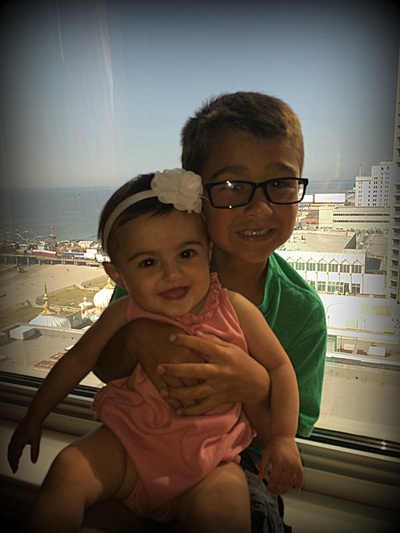
On May 14th, 2013 at 4:11pm and 8:18pm, Jase Nicholas and Milania Maria were born at 23w5d at Lankenau Hospital just outside of Philadelphia. Jase Nicholas was born at 1lb 5.3oz and 12 1/2inches long and Milania Maria at 1lb 2.9oz and 12 1/4inches long. I was admitted there 9 days before on strict bedrest due to bulging waters. Lankenau has a Level 3 NICU and my OB felt I needed to be there though she would not be. The labor and birth were very sad and traumatic because we knew the odds were stacked against our babies. That was nothing compared to what was to come. On Day 2, we lost Jase due to bilateral grade 4 IVH, Pneumothorax and other issues related to his prematurity. On that same day we were told Milania may not make it because she was acidotic and had an irregular heart rhythm. She also had a grade 1 and 2 IVHs but the docs felt confident that they would resolve on their own…the concern was getting her acidosis resolved before they could be damage to her organs .  In the next few days, Milania pulled through and her levels came back to normal with the help of great care and lots of adjustments to her bicarb…then, she needed to be moved to the oscillator vent from the conventional vent. The doctors explained that she had a PDA. Cardiology came in on June 4th and performed an EKG to evaluate her heart and examine the PDA. They determined her PDA was large but wanted to see if they could treat her with a round of Indomethacin right away. The hope was that the Indomethacin would close the PDA because her blood was not oxygenating correctly and it was “flooding her lungs”. We were warned of all the side effects of the Indomethacin, including the increased risk of developing NEC, but we thought it was worth a try to help her breathe better. She was also given Lasix to help dry up the fluid buildup in her lungs due to the PDA. Once the round of Indomethacin was completed (3 doses over the course of 36 hours) the doctors said that they thought her PDA was closing. On June 10th the PDA was wide open again and they prepped her for another round of Indomethacin. On June 13ththe PDA sounded like it was closed again but for some reason Milania was needing more support via the vent and oxygen...she was anywhere from 47-60% oxygen, way up from her normal 21-25%. That night her doc decided to start a 10 day course of steroids to help her get through this latest bump. That first dose gave her a little boost and I saw my pretty little miracle with her eyes open for over an hour for the first time in 12 days…it was bliss. On June 14th the NICU called just as my oldest son was about to walk across the field to receive his high school diploma…they thought Milania was developing an infection. Pure panic insued. Antibiotics were started and cultures were sent to the lab…within 24 hours she seemed to be doing much better thankfully, but her PDA was open…again. Docs decided to wait out the steroid course before doing anything further about her PDA. The steroids likely opened it up again, but due to her breathing support requirements, it was the right choice to start them. On June 16th, we celebrated Father’s Day in the NICU. On June 17th she continued to improve with the help of the steroids and for the first time we saw her face without tape. She had a lot of secretions so her vent tube needed to be retaped. It was the first time we were there for a change and more than a month after our baby girl was born, we finally saw her precious face. Over the next few days, Milania continued to improve…she tried on her first hat, her first bow and I was able to lean into her isolette and kiss her for the first time on June 21st, but her PDA was still open.  She finished her 10 day course of steroids and the docs were happy with her progress. The plan now was to wait a couple weeks and start another course of steroids to extubate. At this point, Milania was now 29 weeks gestation. She was doing so well, the docs were talking about trying an Evita vent which is the same as CPAP but through the ET tube. On June 27th Milania’s belly became distended and she was not able to maintain her temp…our worst fear was becoming a reality…Milania developed NEC…she was still so small at 2lbs 12.2oz. By the next morning things went downhill fast and her docs requested an emergency transfer to a Level 4 NICU, Children’s Hospital of Philadelphia (CHOP). We were beside ourselves. She was on the highest settings possible on the oscillator and on 100% oxygen…and the PDA was still open. Then in came our old friend Acidosis. She was having x-rays and blood gases every 2-4 hours and the docs never left her bedside. The thought was that she would perforate at any minute and need emergent surgery. The goal went from being extubated to just keeping her alive period.  The docs at CHOP worked vigilantly to keep her stable and her blood pressure up. Keeping her blood pressure up would help blood get to her gut…something she desperately needed and the PDA was preventing. Due to her PDA being so large, her blood was shunting the wrong direction and there was limited blood flow to her gut. We did not know this until CHOP did an ultrasound to check her bowels. They were looking for perforations or even bowel death and learned about the blood flow at that time. Milania was extremely critical and the focus had to stay on the NEC…she was treated with Vancomycin, Dopamine, Morphine, Hydrocortisone and Platelets to name a few. Prior to arriving at CHOP she was off all IV fluids and to see her with IVs in every extremity was horrible. Her body had a major inflammatory response to the NEC and she gained 2lbs in fluid over just a couple days…our sweet princess was unrecognizable.  With everything going against her, our little fighter rebounded and was moved back to conventional vent on July 2nd…while she was not being given the Hydrocortisone intravenously for her respiratory support, it inadvertently helped her improve. Over the course of the next few days, Milania was stable but the NEC was not clearing up. The docs decided to consult with Cardiology about her PDA to see if surgery would improve the blood flow to her gut. Throughout the next week things continued to be up and down every day and sometimes changed hourly. Cardiology ordered an EKG and it showed her PDA was very much open…that with the ultrasound of her belly showing limited blood flow and her lack of steady improvement led the docs to say “Uncle” and schedule a PDA Ligation as soon as possible. On July 12th her bedside PDA Ligation was performed. Start to finish the surgery was 40 minutes. The surgeon came to see us and explained that her PDA was “very large” and definitely needed to be addressed. He went on to say that he clipped it twice for good measure. I questioned if her PDA caused her develop NEC. He said that is very much a possibility. There were many more obstacles to come… Milania’s PDA Ligation was just the beginning of her recovery, but without it, she likely would not have survived. Milania went on to have more surgery and defy all odds. She came home from the NICU on Day 144 with an NG tube and ¼ liter of oxygen, but she was home and that was all we ever hoped for. Today she is a happy, healthy 15 month old princess who lights up our every day. On April 6, 2013, my husband and I found out we were expecting our second child. Unlike my first pregnancy, I was super nervous about my pregnancy, even though everything was looking great in the beginning. We found we were having a girl and couldn't be happier. On July 24, 2013, at about 18 weeks pregnant I woke up and quickly realized I was bleeding. I had an ultrasound done and was told I had placenta previa (my placenta was low lying). On August 24, I was bleeding and having contractions so I went into the hospital. Leighton Marie was born on August 31, 2014 weighing 1 lb 10 oz. The staff in the NICU at Women's and Children's Hospital in Mobile, Al was amazing! They were comforting during the hardest time of our family's life. During our 3 1/2 month stay at the NICU, we had a ton of ups and down. There was a lot of taking one step forward but then taking two steps back. Over all Leighton did an amazing job in the NICU. She had one major scare during the first week of her life. Her stomach was extremely swollen. She was very close to having colostomy surgery. If she had the surgery, she would most likely have a colostomy bag on her stomach for the rest of her life. That was a scary time, but I was mostly thankful that she was alive. The doctors ended up finding a plug in her stomach and removed it. I'm very thankful that she does not have to have that health problem for the rest of her life. She, of course, had problems with her breathing, many heart rate drops, and problems with holding her temperature. Our time in the NICU was an extremely trying time but the staff at the NICU, especially the nurses, made it less stressful. We are so thankful for the care they provided our miracle baby girl. She is now a very happy and healthy, just small, almost 1 year old.
 The Other Side of the NICU By Krystal Roark When most people think of the NICU, they think of the miracles that spend days, weeks, or even months growing and fighting, eventually getting those words every NICU parent waits for, "You can take your baby home today." What's rarely thought about, are those littles ones who lost their fight. They aren't any less of a fighter than those who go home, they aren't any less of a miracle either. They just got to go home without their parents. To a whole different home. I had twin daughters in the NICU. Both were amazing fighters. Both died Within 7 days of each other. I went through what all NICU parents feared, twice. I had to plan and attend the funeral of my first daughter,Willow, while Hazel was still in the NICU trying to pull her vent out. I had to grasp at hope, when all I had left of my first born was a memory box. I couldn't even grieve fully. They say that babies in the NICU can pick up on their parents emotions. I didn't want Hazel thinking I gave up on her. I put every ounce of my strength and energy into willing her to live. I had to focus on Hazel going home, not Willow dying. I didn't have time to grieve Willow when I wouldn't leave Hazel's side. 7 days after Willow died my world collapsed in on itself. I experienced both of their losses at once. I felt disconnected from everything. I cried in the arms of the NICU nurses who were crying with me. How do they do it? I know they get attached, I saw it happening with my daughters. When Hazel passed, I heard one nurse immediately call another on her day off. Crying, she told her Hazel passed. In that moment I felt sorry for the nurses of my daughters. I never even thought about how it felt to them. Less than 5 months after my daughters died I found myself shaking like a leaf in the hallway outside the NICU I had memorized. I was holding several NICU care packages I helped put together with Project Sweet Peas' Greater Lafayette Division, Avi's Embrace. I held it together until the maternity ward doors opened and a very familiar nurse walked out and saw me. She had helped care for me in my weeks of hospital bedrest. She immediately started to cry and hugged me asking what I was doing there. My voice shaking, I told her about the NICU care packages and memory boxes I was holding. "God bless you child," she said as she held me. We were escorted down the hall toward the NICU. The doors open and I was overwhelmed. It was too soon. Memories washed over me in a flood. My knees went weak. Then, I was reminded of why I was there. Her. There she was, swiftly walking over to me when the doors opened. Hazel's main nurse. She is one of the many reasons I gave back to the NICU. When a child dies or lives it doesn't just affect the family, it affects their nurses as well. They mourn and rejoice with the family. While my NICU experience wasn't a happy ending, I know the uncertainty that faces every parent that walks through those doors. The moment of hope a small package from another caring parent who's been in your shoes can bring. I know. I just don't know what it's like to take my child home from the NICU. I give back to my NICU in honor of my daughters and their stay and in honor of all those children without a happy ending, who's faith, determination, and courage are often lost in the joy of those coming home. Their stay in the NICU isn't any less important than those who go home. Here's to all those who made it home, if only in our hearts.
I started having labour pains on Friday 16th. Not having a big pain threshold I was scared but as they were only twinges, I thought that it was just braxton hicks. I had developed a cold so felt rough. I snuggled on Jack's sofa and slept most of the weekend. I didn't want to go to hospital just yet, only to be sent home. The pains stayed all weekend. I woke up at 5.30am on the Monday and I was in agony. I was lucky to have my mum there who was fantastic. She made me a hot water bottle, cups of tea's and rubbed my back as I sat on my birthing ball.
I could handle it, so I thought I would only be a few cm dilated after hearing stories of labor. I knew I would be here a while. At 11.10 the pain was worse but i managed. Then something felt weird... my waters went at 12.10pm. My mum phoned the hospital who told us to go to the triage. She also phoned Jack to leave work as the baby was coming! My dad very kindly came home from work to drive me and mum to the hospital. I arrived at the hospital at 12.30pm in agony. As we were waiting for the lift Jack walked through the door, relief ran through me. We went straight up to triage and i was measured. I was 8cm dilated. Wow, i didn't think i would even be 3 cm! They took me through to the labor ward and was checked again. From going to one floor to another I was fully dilated our daughter seemed eager to meet us. Lynne the midwife put me on a heart monitor to check baby's heart beat; great 120 throughout. With Entinox, I was in pain. Lynne checked to see if "anything was happening." Our daughter was born at 2.10pm weighing a great weight at 8lb 11oz. When she was born she wasn't breathing properly. She was purple and made no effort to move or breathe. She had caught an infection- GBS (undetected), because we had not been checked or given anti biotics. She also had Sepsis. She seized a few times and had suffered a H.I.E GRADE2. So a team of fantastic nurses came in inflated her lungs until she was stable enough to move down the NICU. We waited for what seems like ages. Jack was looking pale. He had seen more than what I had. I took his hand and smiled. He knew i was just as scared. He told me she would be perfect and was referring to her as Evie, so we chose to name her Evie - which happens to mean life! The decision to transport her to another hospital for a cooling mat was made pretty quick, roughly 2-3 hours after delivery. We were also told the first 48 hours were crucial and to expect some sort of disability as the cooling mat may not work. They were not sure they were going to make the 7 hour window needed. Evie was going to be transported to the Leeds General Infirmary for the cooling system. Jack and I finally got to meet her at 7.30pm as they were prepping her. She looked so tired. It was hard not to just pick her up and tell her everything would be ok. We stroked her hand for half an hour and then we went back to the labor ward to wait to be discharged. We were very lucky to have Evie when we did as we was the only family on the labor ward between 2pm and 9.30pm when we left. We arrived at 10.30 to see her for a couple of hours. I didn't want to leave her. I cried all the way home but i knew this was the right thing for her. Her Dad and I along with Evie's grandparents visited her everyday. Evie responded well to the treatment so day three the doctors took her off oxygen and slowly throughout the day warmed her temperature back to normal.All the Dr's were amazed to see this little girl who had been through so much, seeming to be pulling through. Day Five Evie was transported back to our local NICU were staff were fantastic at making us feel like even though we had no baby at home we were still mum and dad. Day 7 Evie was allowed to be cuddled... WOW Our first cuddle after 7 days.... WOW, words can not describe how amazing that felt, it was very hard not to squeeze all my love into one cuddle. Then everything seem to go to a halt. She had caught another infection. I was distraught thinking we had come this far and now I was going to lose her. The Dr's were convinced the infection was through the long line IV through her belly button. Later that day they took it out but needed to put the cannula somewhere else as it was doing her medication, so they decided to shave both sides of her head to put a cannula in. They had made her poor little feet look like pin cushions, the nurses couldn't get one in. Luckily they managed again in her foot. Day 12 Evie was discharged from the hospital. Finally I could be Mum! Day 14 Evie was booked in for an MRI to see what the H.I.E had done to her brain. When her consultant phoned he explain that the brain damage was only of the thalamus of the brain, that it was very minor and he was happy with the results as this should not really affect how Evie develops. At nearly three she has been discharged from all care and we are getting ready for her to start nursery. We haven't forgot the fight we all went through, so we set up an awareness page called Get In The Know HIE.
 Items for Baby These items for baby enable parents to care for and bond with their baby. A parent’s touch only accounts for 14% of baby’s interaction in the NICU, which can may lead to a prolonged NICU stay and future complications such as sensory issues. Items for baby also help make the NICU life as "homey" and "warm" as possible. They can bring comfort and hope to both the families and their babies. Eye Masks- These are used to cover the eyes of the infant to allow the baby to rest. Most often hand made with flannel fabric. Blankets- Either handmade or store bought. 16”x20” is an appropriate size for preemie blankets, and approx. 30”x30” for full term. Hats- Knit, crochet, or store bought in preemie or newborn sizes. Round Knifty Knitters are a great tool to use to make quick and easy hats, and can be purchased at Walmart or craft stores. Booties- knit, crochet, or store bought in preemie or newborn sizes. Scratch Mittens- Used to help keep little hands from scratching their face or pulling at wires. Stuffed Animals- For baby to have at bedside it adds a touch of home to the babies isolette. Not all hospitals allow stuffed animals, so please check with your NICU contact before including. Scent Dolls- The parent's scent can aid in bonding with babies in the NICU. These are simple dolls that are made to be worn by the mother next to her skin, and then given to the infant.  Memory Making Items These items give parents the opportunity to capture memories with their new babies, something all new parents want to do. Many babies in intensive care are experiencing serious, life-threatening conditions; therefore, capturing moments with their babies are even more important for parents. These items help families record, remember, and celebrate their new child’s life. For instance, a picture frame can be used to display a picture of the family by the baby at all times or it can be used for the parents to keep and display a picture of their baby so that they have it with them during the times they have to be separated. Isolette Decorations- Small decorations to hang on the baby isolettes. Hand painted wooden decorations and name plaques are commonly used. Birth record pillows are also beautiful keepsakes to include. Disposable Cameras- Used for families who may want to leave the camera with the nurses to capture moments while they are not there. Before donating disposable cameras check with your local NICU to see if they have a camera already available in the unit. Children’s Books- In the NICU parents may not be able to partake in the daily care of the child. Reading to the infant can aid in bonding, and the parent’s voice can be soothing to child. Pick classic stories that are easy to read. Children’s books may also be used for sibling bags. Hand/Foot Print Kits - Enable families to create a precious keepsake together with their baby.  Items for Parents Journals- Used for parents to write down their thoughts, or keep important notes, questions, and terms. Puzzle Books- Puzzle and activity books are included to give parents something to do during the downtime while they sit at the baby’s bedside. Coloring and children activity books can also be used in sibling bags to keep young siblings busy. Tissue Packs- Needed due to the results of the emotional and physical stress of being in a NICU Lotion and Lip Balm- unscented lotions are used for both parents whose hands can be dry from constant sanitizer use, and used in daily care to massage the infant when permitted. Hand Sanitizer- Travel size hand sanitizer is perfect for parents who are constantly in and out of the NICU. Travel Sized Toiletries - During a NICU stay, many families are displaced from their homes. Parents spend many hours of the day with their babies and often do not have items available for personal care. Gift cards (gas, food, lodging, etc.) - Financial hardship is common in the NICU. Not only are parents accruing medical expenses, they often struggle to afford transportation, food and lodging during their stay. Many of these items can be purchased in your local stores. Visit our website to purchase items specially created with families in the NICU in mind. All proceeds from the sale will contribute to grant funding to provide for the financial needs of NICU families.
Shop now: www.nicuawareness.org/store.html |






























 RSS Feed
RSS Feed