|
Your baby may have stayed in the NICU for days, weeks, or even several months. No matter what your NICU experience looked like or how long your journey has been, bringing your little one home is a huge deal. Congratulations! You may be feeling a variety of emotions ranging from joyful and excited to anxious and overwhelmed. All of these feelings are 100% valid and normal. Make sure to reach out to friends and family members who can support you during this emotional time. As the big day approaches, try to become as independent as possible with your baby. The more time you spend feeding, changing, snuggling, and otherwise caring for your baby, the more comfortable and confident you’ll feel when you get home. Specific requirements for discharge may vary depending on your hospital and NICU. If the care team has decided your baby is ready to come home, you know that your baby is medically stable and has also met the following general criteria  1. Consistent weight gain Growth is one of the most important reflections of your baby’s health and development during the first months of life. Your baby is showing a consistent pattern of weight gain if the doctors are discussing sending him/her home soon. If your baby isn’t gaining weight, your medical team may need to either increase their feeding volume or boost their calories by including formula in their diet. Formula has more calories than breastmilk and so it is sometimes necessary to supplement with 1-3 bottles of formula per day to get babies the calories they need to grow – preemies in particular. If you’re breastfeeding and nearing discharge, you’ve hopefully already received guidance and support from a lactation consultant. But, if your breastfed baby is not gaining weight after the first week of life, you’ll want to have a lactation consultant observe a breastfeeding session. 2. Adequate feedings If you’re nearing discharge, your baby is eating well enough to get the calories they need to grow, develop, and thrive. In most cases, this means that your baby is eating all of their food by mouth – either by breast or bottle feeding, or a combination of both. However, some babies may have feeding issues or medical conditions that mean they need to go home with a feeding tube for a few weeks or months in order to safely get the calories that they need. If your baby does need a feeding tube, you will be given all of the necessary equipment and trained on how to manage it at home until you are comfortable and confident. 3. Additional medical needs accounted for It’s not uncommon for some NICU babies to need oxygen support when they first come home from the hospital. If this is the case for your child, you’ll have the appropriate equipment delivered to you and you’ll be taught how to use it before you go home. Your baby may need to have follow-up appointments with specialists for the first months or years after coming home from the NICU. Some common areas that NICU babies often require monitoring of are the: eyes, brain, heart, lungs, digestive system, and skin. Your baby could also have a genetic condition that will need follow-up or a congenital issue that requires future surgery. If your baby will need to have specialist checkups, your medical team will contact those physicians and get these appointments established before you leave the hospital. Remember that eye appointments are especially important. Retinopathy of Prematurity (ROP) is a condition that affects the blood vessels in the eyes of some preemies and can lead to blindness if left untreated. If your baby is a preemie, they were screened for ROP long before discharge and have been receiving regular eye exams to ensure their condition is stable. 4. Car seat test Many NICU babies will need a car seat test before they can leave the hospital. It’s usually done in the last few days before going home. Most preterm and late-preterm infants should have a car seat test, plus those with certain medical conditions or congenital disorders. Specific criteria for needing a carseat test will vary depending on your hospital. A car seat test means that your baby will sit in their car seat for a set amount of time (usually 1.5 - 2 hours) while nurses monitor their vital signs. Some babies may have issues maintaining their oxygen or heart rate while in the car seat, so it’s important for your baby’s safety that any issues are identified before you go home. If your baby fails his/her car seat test, your hospital may provide you with a car bed to use instead. Here are some other important points about car seat safety:
 Feeding Your Baby Most NICU babies, especially preemies, need a bit of extra help and care with feeding. It can sometimes be difficult for babies who are first learning to eat to figure out how to coordinate the ‘suck-swallow-breathe’ pattern that’s required for the baby to safely take milk into the mouth and down to the stomach. Many babies get overly excited while drinking a bottle and will swallow many times in a row while forgetting to breathe. It’s important to always pay attention to your baby while breast or bottle feeding to make sure they’re pacing themselves and taking a breath every 5-6 sucks. If not, you may need to tip the bottle every several swallows so that there’s no milk in the nipple and your baby is forced to pause and breathe. This is called external pacing – if you’re approaching discharge and don’t feel confident with how to do it, ask your nurse to help you practice. This is one reason why it’s so important to spend as much time in the NICU as you can before you go home. You should feed your baby enough times to learn their unique feeding habits – how much they pace themselves, the little things that help them eat better (frequent burping, for example), and what their particular eating patterns are. It’s also helpful to practice feeding while in the NICU without checking the monitor – just your baby. Many NICU parents get so accustomed to the monitor over the course of their baby’s hospitalization that they start to rely on it and watch the monitor during the feedings instead of their baby. Ask your nurse to turn the monitor facing away from you for a few feeds so that you can’t see it if you might find it hard to resist the temptation to look. Watch your baby for signs of distress such as coughing/choking or their skin turning blue or dusky-colored. You'll feel more confident feeding when you get home if you know what you’d see if something was wrong. One really common question is how to tell if your baby is getting enough milk when you’re at home and don’t have nurses closely tracking each feed and weighing your baby daily. A great, objective way to determine feeding adequacy at home is to count the number of wet diapers per day. There are diaper log sheets available online that you can print out and use, as well as apps you can download on your phone or tablet. If your baby isn’t having 6-8 wet diapers per day, he/she may not be drinking enough and could be getting dehydrated. Call your pediatrician to schedule an appointment ASAP. Your pediatrician will also be closely watching your baby’s weight to make sure that they’re growing appropriately, and therefore eating enough. If the nutrition plan is to discharge home from the NICU on formula supplementation, your pediatrician will be the one to determine when is the right time to adjust your baby’s feeding plan. If your baby is gaining good weight, your pediatrician will decide to decrease the calories in your baby’s formula over time and even eliminate formula supplementation altogether. If your baby is going home with a feeding tube, your pediatrician will also be the one to decide how long the tube needs to stay. Helping your Baby Sleep Safely & Soundly It’s critical for your baby’s safety that they sleep in their own simple, dedicated sleeping area, free of any objects that . Adhering to recommended safe sleep guidelines is one of the most important things you can do to reduce the risk of Sudden Infant Death Syndrome (SIDS). According to the American Academy of Pediatrics1, newborns should sleep on their back, alone, with nothing else in the crib. This means no bumper around the edge of the crib, no stuffed animals or toys, no big fluffy blankets or even a hat – just the baby, one layer of clothes, a single sheet, and their swaddle or sleep sack. Besides basic sleep safety, uninterrupted sleep is extra important for NICU babies, especially preemies. Premature babies are born before their brains are fully developed, which can cause them to have sleeping patterns that are slightly different from full-term babies. If your baby is a preemie, he/she may sleep for shorter periods but awaken more frequently and startle more easily than a term infant. Regardless of whether your baby was premature or term, you should do your best to promote uninterrupted, restful sleep as much as possible. Sleeping is when newborns’ most important growth and brain development happens. It comes down to this – if your baby is sleeping comfortably between his/her feeds, don’t bother them. One prime example of this is waking your baby up between feeds to change their diaper. You’ll be doing feedings every 3-4 hours, so it’s best to let your baby continue to sleep and just do the diaper change before the next feed. This doesn’t mean you should avoid picking your baby up and holding them if they’re sleeping soundly in their crib. Your baby will sleep even more peacefully and happily while resting comfortably in your arms. Not to mention, cuddling a sleeping baby is therapeutic for you, too! Noise level is also something to be mindful of in order to help your baby get the sleep he/she needs. Depending on how much time your baby spent in the NICU, he/she may have actually gotten used to the noisy hospital environment. Some parents say that when they finally come home from the NICU, their baby has trouble sleeping in the much quieter and more peaceful home environment! Put a white noise machine or shusher close to the crib and see if it helps your baby sleep better. When to Call for Help Your care team will educate you before you leave the NICU about issues that require medical attention or follow-up. It’s important to understand what requires your immediate action vs. a call to the pediatrician. Supporting your Perinatal Mental Health and Wellbeing The journey of pregnancy, childbirth, and parenting introduces significant transformations to both your life and emotional well-being. The stress, uncertainty, and emotional roller coaster of the NICU experience can cause parents can weigh heavily on parents. If you notice any of these signs, it's crucial to seek help. Reach out to your healthcare provider, or mental health professional. Remember, seeking assistance is a sign of strength and prioritizing your well-being, ensuring you're better equipped to navigate the challenging journey of NICU parenthood and beyond. • You might be feeling down. • You may feel more tired than usual, yet unable to sleep or rest. • You might be less interested in eating. Or eating too much of the wrong things. • You may get angry and annoyed more easily. • You might have trouble thinking clearly and making decisions. • You may worry or get anxious for reasons that you don’t completely understand. • You might be having thoughts or impulses that feel disturbing, scary, and irrational. • You may even experience flashbacks or nightmares about past traumatic events. All these reactions are normal, but they may also be signs and symptoms of a temporary and treatable set of conditions called Perinatal Mood and Anxiety Disorders (PMADs). For resources, please visit: https://www.nationalperinatal.org/mental-health As the big day approaches, remember how far you and your family have come on your journey. You are strong, resilient, and amazing, and you’ve already made it through the most difficult part. Remember to try to take time for self-care in the midst of daily life with a newborn – even if just 10 minutes a day. You need to take care of yourself mentally, emotionally, and physically in order to take the best care of your little one. I think I can safely speak for your nurses when I say – send us a note sometime down the road to let us know how you and your family are doing! It’s the ultimate reward for a NICU RN to see former patients thriving years later as adorable, happy children. Once again, congratulations! About the AuthorBailey Deal, RN is a neonatal nurse at one of the top-ranked children's hospitals in the United States. When not at work caring for babies, she’s a freelance health writer and blogger at www.babynursebailey.org. References
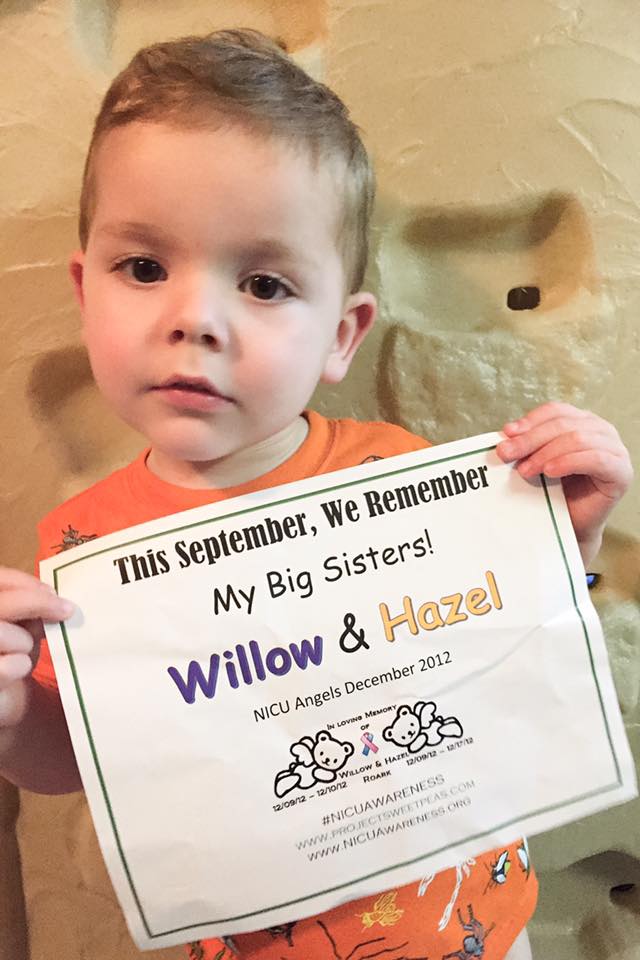
https://www.nationalperinatal.org/mental-health https://www.aap.org/en/news-room/news-releases/aap/2022/american-academy-of-pediatrics-updates-safe-sleep-recommendations-back-is-best/  It's a terrifying moment when your baby needs to be in the Neonatal Intensive Care Unit (NICU). It's overwhelming and can be downright devastating. Admission to the NICU may be completely unexpected, or you are already aware that your baby will require intensive care after birth. Either way, it is a scary and stressful situation. There is so much fear of the unknown. What will happen to your baby? Who will be caring for them? When can you see your baby? The questions and concerns are endless. Your NICU team is your ally, and they are that guiding hand of support you will reach out to for the following days, weeks, or even months. The neonatologists, respiratory therapists, dieticians, social workers, and nurses are the experts who will help you through this difficult time. Your NICU nurses are with your baby all day and all night. They are like guardian angels and are the advocates you will be closely working with during your time in the NICU. Here are 5 things that your NICU nurses want you to know: |

























 RSS Feed
RSS Feed